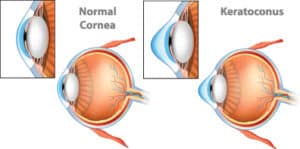
 Keratoconus is a progressive eye condition that occurs when the cornea, which is usually dome-shaped, thins and bulges outward. The condition significantly impacts quality of vision, meaning vision correction is a necessity in most cases. However, correcting vision can be challenging with keratoconus and requires a tailored approach. This is why the experts at Laser Eye Center of Miami offer several options for treating keratoconus. These safe and effective solutions are designed to improve vision and quality of life for keratoconus patients.
Keratoconus is a progressive eye condition that occurs when the cornea, which is usually dome-shaped, thins and bulges outward. The condition significantly impacts quality of vision, meaning vision correction is a necessity in most cases. However, correcting vision can be challenging with keratoconus and requires a tailored approach. This is why the experts at Laser Eye Center of Miami offer several options for treating keratoconus. These safe and effective solutions are designed to improve vision and quality of life for keratoconus patients.
Stages of Keratoconus
Keratoconus advances at varying rates, depending on the patient. It can also progress differently in each eye. Cases in which keratoconus develops early are associated with a more rapid progression of the condition.
Early keratoconus: Early-stage keratoconus comes with a slight impact on vision. Glasses and soft contact lenses are typically useful in correcting vision at this stage.
Moderate keratoconus: Patients may begin to notice corneal changes at this stage. Vision quality starts to decrease, even with glasses.
Advanced keratoconus: In advanced keratoconus, corneal scarring appears, and the conical shape of the cornea becomes more obvious.
Severe keratoconus: Quality of vision is severely degraded at this stage, which is also characterized by scarring and thinning of the cornea. Patients may not be able to tolerate contact lenses, due to the irregular shape of the cornea.
Fortunately, there are several treatment options available to patients with keratoconus.
Specialized Contact Lenses
 As the cornea becomes more cone-shaped, glasses and soft contact lenses become ineffective at providing substantial vision correction. Certain contact lenses can help patients see more clearly with advanced-stage keratoconus, including:
As the cornea becomes more cone-shaped, glasses and soft contact lenses become ineffective at providing substantial vision correction. Certain contact lenses can help patients see more clearly with advanced-stage keratoconus, including:
Rigid gas-permeable lenses: These contact lenses can be customized to the unique shape of the protruding cornea. Additionally, they are easy to place, remove, and maintain, making this a viable option for many patients.
Scleral lenses: The large diameter of the scleral lens provides coverage to the entire cornea, resting on the sclera.
Corneal Collagen Crosslinking Corneal Transplant
Corneal crosslinking is an advanced therapy that is effective at slowing or completely inhibiting the effects of keratoconus by treating the weakened cornea. During this procedure, one of our experts will first administer vitamin B eye drops into the eye before shining a special light onto the cornea. This combination makes it possible for new collagen cross-links to develop, resulting in a stronger cornea.
Intracorneal Ring Segments
Intracorneal rings are small plastic half-disks that are placed into the cornea to help flatten its irregular shape caused by keratoconus. These devices do not stop the progression of keratoconus but may make it easier for patients to better tolerate vision-correcting contact lenses. Other treatments are needed to stabilize the cornea.
Corneal Transplant
When other treatments have been ineffective, keratoconus patients may be eligible for a corneal transplant. During this procedure, the existing cornea is removed and a donor cornea is securely placed. After corneal transplant surgery, glasses or contact lenses will likely still be needed to achieve crisp vision.
FAQs
What Causes Keratoconus to Develop?
Keratoconus occurs when the cornea thins and bulges into a cone-like shape, leading to distorted vision. While the exact cause isn’t always clear, several factors may contribute to its development. Genetics play a significant role, meaning if you have a family history of keratoconus, you could be at higher risk. Environmental and lifestyle factors, such as excessive eye rubbing or chronic eye irritation, may also contribute to the condition’s progression.
How Is Keratoconus Diagnosed?
Early detection is key to managing keratoconus effectively. An eye specialist can diagnose keratoconus through a comprehensive eye exam, including corneal topography, which maps the cornea’s shape, and pachymetry, which measures corneal thickness. If you notice sudden vision changes or increasing difficulty with corrective lenses, seeking an evaluation can help determine if keratoconus is the cause.
Can Keratoconus Be Cured or Reversed?
Currently, there is no cure for keratoconus, but effective treatments can slow its progression and improve vision. Advanced options like corneal cross-linking help strengthen the cornea and prevent further thinning. In more severe cases, specialty contact lenses or corneal transplant surgery may be necessary. Seeking treatment early can significantly improve long-term outcomes.
What Lifestyle Changes Can Help Manage Keratoconus?
While medical treatment is crucial, certain lifestyle habits can help manage keratoconus symptoms. Avoiding excessive eye rubbing is essential, as it can weaken the cornea and accelerate progression. Protecting your eyes from UV exposure by wearing sunglasses and keeping your eyes hydrated with artificial tears can also help maintain eye health. Additionally, following up regularly with your eye specialist ensures timely intervention if your condition worsens.
Can Eye Rubbing Contribute to Keratoconus?
Yes, frequent or aggressive eye rubbing can contribute to the development and worsening of keratoconus. The repetitive mechanical stress on the cornea can weaken its structure, making it more susceptible to thinning and bulging. If you have allergies or dry eyes that cause irritation, using prescribed eye drops instead of rubbing your eyes can prevent unnecessary damage.
What Is the Success Rate of Corneal Transplants for Keratoconus?
For advanced keratoconus cases where other treatments are ineffective, a corneal transplant may be necessary. This procedure has a high success rate, with most patients experiencing significantly improved vision post-surgery. Advances in transplant techniques have increased the likelihood of long-term graft survival, making it a reliable option for severe cases. However, as with any surgery, risks such as graft rejection or infection must be considered.
Are There Any Risks or Side Effects Associated With Keratoconus Treatments?
Keratoconus treatments are generally safe, but they do carry some risks. Corneal cross-linking may cause temporary discomfort, light sensitivity, or mild inflammation, though these effects typically subside within a few weeks. Corneal transplants, while highly successful, require a longer recovery period and carry a small risk of rejection or infection. Your eye specialist will discuss the best treatment plan tailored to your condition and risk factors.
How Long Does It Take to Recover From Keratoconus Treatments Like Cross-Linking or Corneal Transplant?
Recovery time depends on the treatment. Corneal cross-linking typically requires a few weeks for the eyes to heal, with vision stabilizing over several months. Corneal transplant recovery can take several months to a year, as the eye adapts to the new tissue. Regular follow-up visits and post-treatment care are essential to ensure the best possible outcome.
Contact Us
For more information about keratoconus treatment options or to schedule a consultation, contact our office or fill out the online form.






